THE CONTEXT: The health sector being a crucial arena of discussion at G20 Summit 2023 held in Delhi, the Prime Minister launched the sixth edition of One Earth and One Health Advantage Healthcare India 2023, where he reinstated India’s vision and commitment towards universal health coverage not just for humans but for their entire ecosystem. Although the initiatives are laudable, however, in order to achieve the objective of one health and universal health coverage it is necessary to focus on primary health care. This article analyses various aspects of primary healthcare in India from the UPSC perspective.
STATUS OF NONCOMMUNICABLE DISEASES (NCDS) AND RELATED INITIATIVE
- Noncommunicable diseases (NCDs), also known as chronic diseases, tend to be of long duration and are the result of a combination of genetic, physiological, environmental and behavioural factors.
- India is experiencing a rapid health transition with a rising burden of Non-Communicable Diseases (NCD) surpassing the burden of Communicable diseases like water-borne or vector borne diseases, TB, HIV, etc.
- The four major NCDs are cardiovascular diseases (CVDs), cancers, chronic respiratory diseases (CRDs) and diabetes which share four behavioural risk factors – unhealthy diet, lack of physical activity, and use of tobacco and alcohol.
- A study ‘India: Health of the Nation’s States – The India State-Level Disease Burden Initiative in 2017’ by Indian Council of Medical Research (ICMR) estimated that the proportion of deaths due to NCDs in India have increased from 37.9% in 1990 to 61.8% in 2016.
- Recently, the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) programme has been renamed National Programme for Prevention & Control of Non-Communicable Diseases (NP-NCD) for widening coverage and expansion.
- Now, the NP-NCD Scheme subsume all types of NCDs with an addition of diseases to the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS), such as non-alcoholic fatty liver disease, chronic kidney disease etc.
GOVT POLICY AND SCHEMES RELATED WITH PRIMARY HEALTH CARE:
- Health and Wellness Centres (HWCs): HWC are created under Ayusham Bharat Programme by converting the existing primary health centres and subcentres. They provide comprehensive primary health care (CPHC) including a child and maternal health services, non-communicable diseases, and also diagnostic services, and free essential drugs.
- Primary Health Centre (PHC): Under the National Health Mission (NHM), Primary Health Centre (PHC) are established to cover a population of 30,000 in rural areas and 20,000 in hilly, tribal and desert areas. PHCs are established to cover defined population.
- Janani Shishu Suraksha Karyakaram (JSSK): The scheme is to benefit pregnant women and infant who access Government health facilities for their delivery and post-delivery care.
- Saksham Anganwadi and Poshan 2.0: It seeks to address the challenging situation of malnutrition among children up to the age of 6 years, adolescent girls (14-18 years) and pregnant and lactating women. The scheme is open to all eligible beneficiaries and the only pre-condition is that the beneficiary has to be registered at the nearest Anganwadi centre with Aadhaar identification.
ONE EARTH AND ONE HEALTH ADVANTAGE HEALTHCARE INDIA 2023:
- One Earth One Health is a holistic approach that emphasizes the interconnectedness of human, animal, and environmental health.
- Recently, the sixth edition of One Earth and One Health has been launched for universal health coverage not just for humans but for their entire ecosystem. It aligns with India’s G20 Presidency theme of ‘One Earth, One Family, One Future’.
- It was organised in partnership with the Federation of Indian Chambers of Commerce & Industry (FICCI), the Ministry of Health & Family Welfare.
- Its primary objective is to showcase India’s competence in the medical value travel industry as a provider of Value-Based Healthcare services and exporter of Healthcare Workforce.
COMMUNICABLE DISEASES
Communicable diseases are illnesses caused by viruses or bacteria that people spread to one another through contact with contaminated surfaces, bodily fluids, blood products, insect bites, or through the air. There are many examples of communicable diseases. Some examples of reportable communicable disease include HIV, hepatitis A, B and C, measles, salmonella, measles, and blood-borne illnesses.
- State of Communicable Diseases in India:
India, a country with a population of over 1.3 billion, has made significant strides in various facets of healthcare. Yet, communicable diseases remain a looming challenge, causing a substantial number of deaths and illnesses annually. From diseases like tuberculosis, which has long haunted the nation, to more recent challenges like the dengue and chikungunya outbreaks, India’s battle against infectious diseases is ongoing.
OVERVIEW OF PRIMARY HEALTHCARE IN INDIA
Primary Healthcare: The First Line of Defense
Primary health care (PHC) refers to a broad range of health services provided by medical professionals in the community. This means universal health care is accessible to all individuals and families in a community.
General health-care practitioners, nurses, pharmacists, and allied health-care providers are exclusive components of the primary health-care team. Basically, the PHC service is the process and practice of immediate health services, including diagnosis and treatment of a health condition, support in managing long-term health care, including chronic conditions such as diabetes. PHC also includes regular health checks, health advice when an unhealthy person seeks support for ongoing care.
With a vast rural populace and dense urban settlements, primary healthcare becomes even more significant for India. It’s not just about treating diseases but preventing them, educating the public, and ensuring early intervention.
Effective PHC systems are characterized by the following:
- Accessibility:PHC facilities should be accessible to all members of the community, regardless of their income or social status.
- Affordability:PHC services should be affordable to all members of the community.
- Quality:PHC services should be of high quality, and PHC workers should be skilled and knowledgeable.
- Comprehensiveness:PHC services should be comprehensive and include preventive care, curative care, and rehabilitative care.
Why Strengthening Primary Healthcare is Imperative
While tertiary healthcare institutions, like specialized hospitals, play a role in treating advanced stages of diseases, the importance of primary healthcare cannot be overstated.
In a country as vast and diverse as India, the eradication of communicable diseases necessitates a bottom-up approach, where Primary Healthcare Centers (PHCs) become the epicenters of change.
By bolstering our primary healthcare systems, we can ensure that every Indian, regardless of their socio-economic background or geographical location, has access to timely and effective medical care.
GLOBALIZATION AND THE SPREAD OF DISEASE
In the age of globalization, the world has become a smaller place. Borders are more porous, and people, goods, and services move across countries with ease. While this brings countless benefits, it also comes with its share of challenges, particularly in the realm of health. Communicable diseases, which once were localized, can now spread globally within days, as evidenced by recent pandemics.
- The Indian Context: Localized Spreading
For a country like India, with its diverse landscapes, dense urban settlements, and vast rural expanses, the concept of ‘local globalization’ is especially pertinent. A disease outbreak in one part of the country can quickly spread to other parts, given the high mobility of the population. This inter-state and inter-district transmission can be likened to global disease transmission but on a national scale.
THE SWOT ANALYSIS OF INDIA’S PRIMARY HEALTHCARE IN ADDRESSING COMMUNICABLE DISEASES
STRENGTHS
- Vast Network of Healthcare Centers: India boasts a vast network of primary healthcare centers (PHCs), sub-centers, and community health centers (CHCs) spread across the country, reaching even the remotest regions.
- Diverse Healthcare Workforce: From ASHA workers to specialized doctors, the healthcare workforce in India is diverse, ensuring varied expertise at the grassroots level.
- Government Initiatives: Over the years, the Indian government has launched various health schemes like Ayushman Bharat, which focus on making healthcare accessible to all.
- Traditional Medical Knowledge: India’s rich heritage in traditional medicine, including Ayurveda, Siddha, and Unani, offers alternative methods for disease prevention and treatment.
WEAKNESSES
- Infrastructure Gaps: Many PHCs and CHCs lack adequate infrastructure, from basic amenities to specialized equipment.
- Staff Shortages: Vacant positions, especially in rural areas, make it challenging to deliver consistent healthcare services.
- Inadequate Training: While the workforce is vast, there’s often a gap in training, particularly in understanding and managing emerging diseases.
- Lack of Technology Integration: Modern health technologies, including telemedicine and health informatics, are yet to be fully integrated into primary healthcare.
OPPORTUNITIES
- Digital Health: With the rising penetration of smartphones and internet connectivity, there’s immense potential for digital health solutions, from remote consultations to health apps.
- Public-Private Partnerships (PPPs): Collaborations between the government and private entities can bring in investments, expertise, and innovative healthcare delivery models.
- Community Engagement: By involving communities in health decision-making, there’s potential for more tailored, effective health interventions.
- Global Collaborations: Partnerships with international health bodies can bring in global best practices, funding, and expertise.
THREATS
- Emerging and Re-emerging Diseases: New diseases, like COVID-19, or the resurgence of old ones, like tuberculosis, pose constant challenges to primary healthcare.
- Climate Change: Altered weather patterns can lead to the spread of vector-borne diseases, challenging existing healthcare strategies.
- Healthcare Funding Cuts: Economic challenges might lead to reduced healthcare budgets, impacting service delivery.
- Socio-cultural Barriers: Misinformation, superstitions, or resistance to certain medical practices can hinder effective disease management at the grassroots level.
CONSEQUENCES OF NEGLECTING PRIMARY HEALTHCARE
Primary healthcare (PHC) forms the bedrock of a nation’s health system. Serving as the first point of contact for individuals with the healthcare system, its role is pivotal in disease prevention, health promotion, and timely intervention. A neglected primary healthcare system can have dire consequences, ranging from health to socio-economic impacts.
RISE IN DISEASE TRANSMISSION
- Without robust PHC systems, routine immunization drives can suffer, early disease detection can be compromised, and timely interventions can be delayed.
- According to a WHO report from 2021, disruptions in essential health services due to the COVID-19 pandemic could result in an additional 200,000 child deaths and 12,000 maternal deaths every month globally. Much of these deaths can be attributed to weakened primary healthcare services.
ECONOMIC IMPLICATIONS
- Loss in Productivity: Sick employees or those taking care of sick family members can lead to reduced working hours and absenteeism. A study published in Health Affairs in 2020 estimated that absenteeism due to illness can cost the global economy around $530 billion annually.
- Increased Healthcare Costs: With a compromised PHC, there’s a higher reliance on tertiary care, which is often more expensive and may involve advanced treatments due to delayed interventions resulting in high out of the pocket expenditure. According to the World Bank, India spends less than 2% of its GDP on healthcare. This is one of the lowest levels of healthcare spending in the world. As a result, many people in India are unable to afford to access healthcare services.
SOCIAL IMPLICATIONS
Disruption of Communities: High disease prevalence can lead to stigmatization, loss of workforce, and even community displacement in extreme cases. Tuberculosis (TB) remains a significant concern in India.
- In 2020, the Global Tuberculosis Report cited an estimated 2.64 million TB cases in India. Neglected PHC can result in delayed TB diagnosis, thereby affecting community health. Stigmatized diseases can lead to reduced social interactions, community cohesion loss, and even mental health issues.
- According to the National Sample Survey, the poorest 20% of the population in India accounts for only 9% of total healthcare spending. The richest 20% of the population, on the other hand, accounts for 42% of total healthcare spending. This means that the poorest people in India are less likely to be able to afford healthcare services than the richest people in India.
Impact on Families: Families bear the emotional, financial, and physical burden of caring for sick members. As per a report by the World Economic Forum in 2021, families in Southeast Asia, including India, spent approximately 7.3% of their monthly income on healthcare, a number that escalates with weak PHC.
CHALLENGES IN NAVIGATING THE COMPLEX LANDSCAPE OF PRIMARY HEALTHCARE IN INDIA
LIMITED RESOURCES AND FUNDING
- Despite the vastness of the healthcare system, funding remains a pivotal concern. The allocation for healthcare in India’s budget, as a percentage of GDP, has historically been low (less than 2%) compared to global standards.
- Underfunded PHCs also result in compromised services, lack of essential medications, inadequate diagnostic tools, and sub-par infrastructure.
GEOGRAPHICAL AND CULTURAL BARRIERS
- India’s diverse terrain, from hilly regions to remote villages, poses logistical challenges. Additionally, cultural differences, language barriers, and traditional beliefs can influence healthcare-seeking behavior.
- These barriers can lead to delayed treatments, reluctance in adopting preventive measures, and non-adherence to medical advice.
OVERBURDENED PHCS
- With the population surge and the increasing burden of both communicable and non-communicable diseases, PHCs often cater to more patients than their capacity allows.
- Overcrowding lead to reduced consultation times, long waiting periods, and potential misdiagnoses. Furthermore, healthcare workers under continuous stress are more prone to burnout.
TRAINED MEDICAL PERSONNEL
- The demand for skilled healthcare professionals, particularly in rural areas, outstrips the supply. Specialized training for emerging diseases is also lacking. This gap can lead to mismanagement of diseases, reliance on under-qualified personnel, and decreased trust in the healthcare system.
FRAGMENTED HEALTHCARE DATA AND LACK OF INTEGRATION
- The Indian healthcare system often operates in silos, with limited integration between primary, secondary, and tertiary care. Additionally, there’s a lack of unified health records. Fragmented data can hinder effective disease tracking, lead to repetitive diagnostic tests, and impede coordinated care.
RESISTANCE TO MODERN MEDICAL INTERVENTIONS
- Misinformation, fuelled in part by myths, superstitions, and occasionally mistrust of modern medicine, poses hindrance to effective primary healthcare. Resistance can manifest in various ways, from vaccine hesitancy to reluctance in seeking timely medical interventions.
SUPPLY CHAIN INEFFICIENCIES
- The timely availability of essential drugs, vaccines, and medical equipment can be compromised due to logistical issues, bureaucratic delays, or inadequate storage facilities. Inefficiencies can lead to stock-outs, hampering disease treatment and prevention efforts.
GOVERNANCE: THE BEDROCK OF EFFECTIVE DISEASE CONTROL
The rapid spread of diseases places an enormous responsibility on governance structures. Effective governance doesn’t just imply a reactive approach to outbreaks but necessitates a proactive stance, focusing on prevention, early detection, and rapid response.
Primary health infrastructures play a pivotal role in either curbing or exacerbating the spread of diseases. On the one hand, robust local health systems can quickly identify and contain outbreaks, reducing transmission rates. On the other hand, weak systems can result in delayed responses, furthering the spread and complicating treatment efforts.
Lack of foresight, underfunded health initiatives, and inadequate infrastructure can result in uncontrolled disease proliferation. Not only does this strain already overburdened healthcare systems, but it also leads to economic repercussions, hampers development, and erodes public trust in authorities.
Governance in healthcare isn’t merely about allocating funds or building infrastructure; it’s about orchestrating a symphony of diverse functions, stakeholders, and resources towards a unified goal of disease control and improved public health.
- The Indian Duality: Central vs. State Governance: India’s federal structure necessitates a delicate balance between central and state healthcare policies. While the central government provides overarching guidelines and support, the implementation largely falls on state governments, each contending with unique demographics, health challenges, and resources.
- The Role of Local Self-Governance Bodies: Panchayati Raj Institutions (PRIs) and urban local bodies play a pivotal role in health governance at the grassroots level. Their on-the-ground presence, understanding of local issues and direct engagement with communities make them instrumental in driving localized health initiatives.
The Analysis:
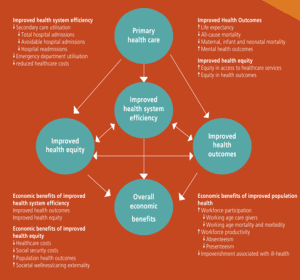
Continuous and comprehensive care provided by the primary health care team can provide effective health education and prevention interventions based on the medical and social needs of patients. This helps tackle risk factors and other social determinants of health, which in turn improves equity of health outcomes.
Drawing on these efforts to strengthen primary health care, efforts by states and the central government in India have been growing. At the state level, many have adopted varied models of primary health care like mohalla clinics in Delhi, Basti Dawakhana in Telangana, Apala dawakhana in Mumbai, and so on.
Nevertheless efficient and fully functionally primary health care facilities are distant in all regions. Neoliberalism and privatisation is to blame as proliferation of private hospitals and private clinics have drawn patients away from the public health system. In urban areas this phenomenon is prevalent although it has begun penetrating rural regions too.
This has led to a shift in focus from primary health care and the public health system to private health care. Efforts and strategic advancement is required to reinstate the importance and efficient working of primary health centres in the public health system.
THE WAY FORWARD TOWARDS ROBUST HEALTH GOVERNANCE:
- Political Will: The commitment of policymakers to address pressing health challenges. It translates into budgetary allocations, policy prioritizations, and the creation of a conducive environment for healthcare reforms.
For instance, India’s commitment to eradicating polio, which was realized in 2014, was underpinned by political will. Leaders across the spectrum recognized the importance of the issue and mobilized resources accordingly.
- Collaboration: Collaborative federalism ensures that health policies are not only universally designed but are also locally relevant. However, it also necessitates greater communication and coordination between the two levels of government to prevent duplication of efforts and ensure the best use of resources.
For instance, The National Health Mission (NHM) is a central government initiative, but its execution is tailored by state governments based on regional health challenges.
- Increased cooperation of International Organizations and NGOs: International organizations (like WHO, UNICEF) and non-governmental organizations (NGOs) complement the efforts of the government. They bring in expertise, funds, and global best practices.
For instance, The WHO played a pivotal role in India’s battle against tuberculosis, providing technical assistance, monitoring, and evaluation. Similarly, NGOs such as the Bill & Melinda Gates Foundation have contributed significantly to various health campaigns in the country. India should reap the benefits of such cooperation ensuring that India’s health initiatives are in line with global standards and benefit from international experiences.
- (Awareness, Investment and Rethinking) AIR Strategy: Awareness to bring back people’s knowledge about the importance of an efficient primary health care structure.
Investment in this domain is the need of the hour. Considering the staggering importance of a primary health centre, it is crucial to have a uniform, mandatory and enthusiastic investment in the primary health structure to overcome the health challenges faced by the country. Without uniformity, a strengthening of the primary health system and universal health coverage is not possible.
Need to rethink and reassess the primary health care needs of the community. The current primary health care system in India follows the guidelines outlined by the Bhore Committee report of 1946. People, society and health care challenges have transitioned over the years. Today the health care needs of the people are different from what people in post-partition India required.
BEST PRACTICES
Kerala’s Community-Based Approach: Kerala stands out for its robust public health system. The state adopted a community-based approach, actively involving local governing bodies and leveraging a network of community health workers. The state boasts high literacy rates, low infant and maternal mortality rates, and has been at the forefront in managing various health crises effectively, including the Nipah virus outbreak and COVID-19.
Tamil Nadu’s Health System Strengthening: Tamil Nadu has invested in strengthening its health infrastructure, including establishing well-equipped PHCs, introducing electronic health records, and ensuring a regular supply of medicines through the Tamil Nadu Medical Services Corporation. The state consistently ranks high in healthcare indices, with reduced mortality rates and efficient disease management systems.
THE CONCLUSION: Despite commendable government initiatives, India’s primary healthcare system requires augmented focus. While strides have been made, many areas, especially rural regions, still face infrastructural deficits, shortage of medical professionals, and inadequate facilities. Fortifying primary healthcare isn’t just a necessity; it’s a cornerstone for achieving comprehensive nation building. SDG 3, which aims to ensure health and well-being for all, underscores the importance of universal health coverage, including quality primary healthcare. Meeting SDG targets is not merely about global commitment but also about ensuring holistic well-being for India’s vast populace. Strengthening primary healthcare is pivotal in this quest.
Mains Practice Questions:
Q.1 The effective and timely implementation of well-designed primary healthcare policies result in improved health outcomes. Comment.
Q.2 What are the challenges faced by Primary Healthcare in India? Discuss the Awareness, Investment and Rethinking (AIR) strategy for improving the efficacy of the primary healthcare services in India.
Additional Information