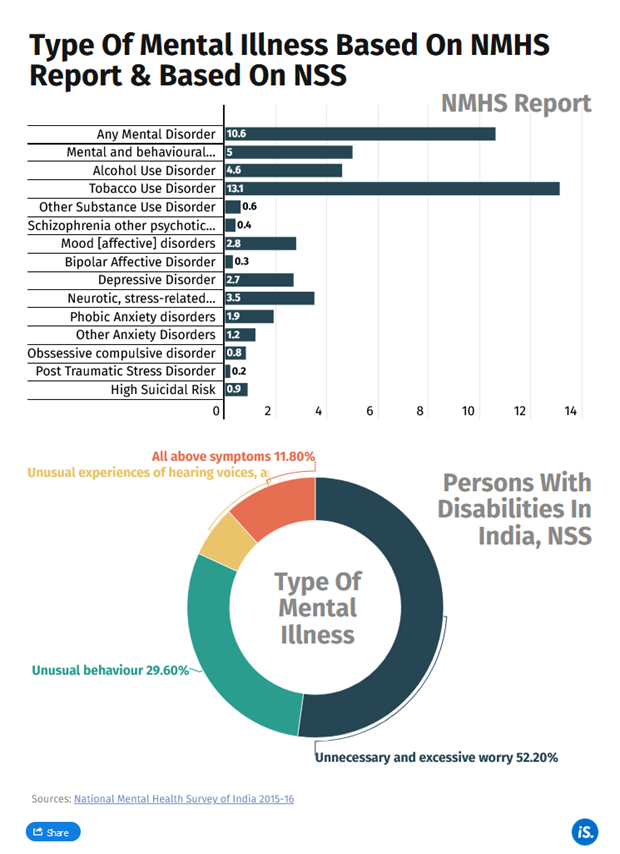
In 2016, the National Mental Health Survey by the National Institute of Mental Health and Neuro Sciences, estimated that about 10.6% of India’s population, above 18 years, lived with a mental health condition.
The National Sample Survey defined mental illness as “a substantial disorder of thinking, mood, perception, orientation or memory that grossly impairs judgement, behaviour, capacity to recognise reality or ability to meet the ordinary demands of life”.
On average, the 2023 study found, Rs 2,115 is spent each month on healthcare by a household, if a member has a mental illness. This adds up to 18.1% of the household’s monthly expenditure. Among the richest households, the monthly expenditure is Rs 3,754, but the burden is highest among the poorest households, where a quarter of the monthly expenditure is on healthcare.
According to National Sample Survey 2017-’18, the average cost of hospitalisation for psychiatric and neurological ailments was Rs 26,843, with an average cost of Rs 7,235 for care in public hospitals and Rs 41,239 for private hospitals. This is comparable to costs associated with cardiovascular ailments.
The expense on mental healthcare includes both direct costs and indirect costs. The amount spent on treatment, medication, travel to hospitals and the like are direct costs. Indirect costs include the monetary value of loss of productivity of patients or caregivers, and intangible costs in terms of stress, stigma and more, borne by those affected.
A study finds how out-of-pocket expenditure has pushed households, with members who have a mental illness, below the poverty line. About 20.7% of these households fall below the poverty line because of healthcare expenses. Among rural households, 22.5% were pushed from being non-poor initially to below poverty line, compared to 17% of urban households.
Suppose you are the Chief Medical Officer of a district, then,
a) What will be your view on the socio-psychological and economic impact of mental illness?
b) What are the ethical issues in the case?
c) What course of action will be taken by you in the district to minimise the socio-psychological and economic impact of mental illness?
Answer:
The Context: The National Sample Survey defined mental illness as “a substantial disorder of thinking, mood, perception, orientation or memory that grossly impairs judgement, behaviour, capacity to recognise reality or ability to meet the ordinary demands of life”, but it does not include “retardation, which is a condition of arrested or incomplete development of mind of a person”.
In 2016, the National Mental Health Survey by the National Institute of Mental Health and Neuro Sciences, estimated that about 10.6% of India’s population, above 18 years, lived with a mental health condition.
a) Socio-psychological and economic impact of mental illness:
Socio-psychological impact
1. Loss of worth-fulness: People will have a sense of worthlessness in life as they have social-psychological problem and a feeling of low confidence.
2. Social stigma associated with mental illness deters patient to seek professional help.
3. Some people with mental health conditions will feel a sense of isolation and disconnection from their communities.
4. Mental health conditions can place pressure on relationships. It demands more understanding from the family members of the patients.
5. Over 90% of psychiatric patients in India live with their families, causing much stress to the caregiver. The caregiver is under considerable stress because of the physical and emotional caregiving along with the social isolation, financial difficulties and troublesome behaviour of the patient.
6. Chronic mental illness in a nuclear household disrupts daily life and drains family resources.
7. Women caregivers face challenges in balancing caregiving, career, child rearing, and household chores, and are less likely to receive informal support for psychiatric treatment.
Economic impact
• A higher proportion of people with mental illness are of the economically productive age group of 19-55 years. This not only reduces their productivity but also leads to economic loss to the country. According to WHO, the economic loss due to mental health conditions in India, between 2012-2030, is estimated at $1.03 trillion.
• Since mental illness typically requires outpatient care and is not covered under insurance in most cases, it is an additional burden on family resources.
• Out-of-pocket expenditure pushes households, with members who have a mental illness, below the poverty line. According to studies, among rural households, 22.5% were pushed from being non-poor initially to below poverty line, compared to 17% of urban households.
The mental disorder result
b) Ethical issues in the case are as follows:
1. Right to health: Due to various factors, people are not able to enjoy their right to health and a healthy life.
2. Poor human capability: Amartya Sen’s Capability Approach says that human capability suffers due to poor health and education.
3. DPSP role of the state: State has responsibility to provide good health facilities but overall health expenditure in India is very low.
4. Due to lack of empathy towards the mentally ill patients, people do not care about them even including family members in many cases. It is also due to lack of knowledge and awareness about mental disorders among the general populace.
5. The growing stress among the youth due to modern lifestyle, unhealthy competition, pressure to perform etc. which is taking a toll on mental health.
6. Breach of confidentiality: The patient–physician relationship is bound by the moral and ethical sanctity of confidentiality, more so in mental health. This is one of the fundamental responsibilities of the psychiatrist. In clinical practice, however, in certain situations, the PWMI themselves waive-off this confidentiality clause.
7. Socio-psychological and economic impact on family members of patients as treatment for mental illness can be emotionally and economically draining.
c) Actions to minimise the socio-psychological and economic impact of mental illness:
Guiding ethical values and principles
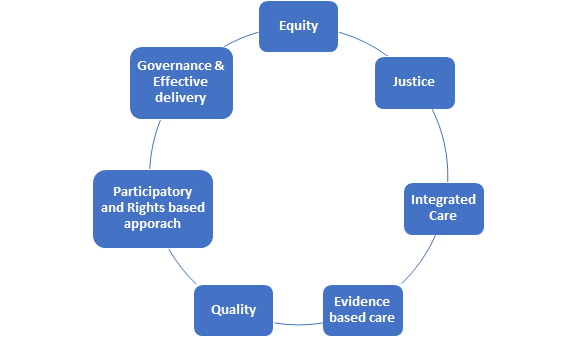
- Implementation of the District Mental Health Programme (DMHP) component of the National Mental Health Programme (NMHP). Facilities made available under DMHP at the Community Health Centre (CHC) and Primary Health Centre (PHC) levels, include outpatient services, assessment, counselling/ psycho-social interventions, continuing care and support to persons with severe mental disorders, drugs, outreach services, ambulance services etc.
- Training can be provided by Medical Officers posted at district hospital to Community health workers and grass root level.
- Arrange periodic mental health camps at village and block level where screening by Medical Officers can be done and if required, referral can be given to the District Hospital.
- Ensure availability of sufficient essential drugs in every PHC, CHC and District Hospital.
- Setting up of a 24/7 helpline to provide psychosocial support, by mental health professionals, to the entire affected population, divided into different target groups viz children, adult, elderly, women and healthcare workers.
- Providing tele-consultation services as part of National Tele Mental Health Programme.
- Issuing advisories on management of mental health issues, catering to different segments of the society.
- Advocacy through various media platforms in the form of creative and audio-visual materials on managing stress and anxiety, and promoting an environment of support and care for all.
- To generate awareness among masses about mental illnesses Information, Education and Communication (IEC) activities can be done in the community, schools, workplaces, with community involvement.
- Imparting life skills to school students through trained teachers and appoint counsellors in colleges.
Conclusion:
Not all impacts of mental health conditions are negative. Living with a mental health condition can enable people to build strengths and skills that support them in their recovery. While the impacts of mental health conditions may be significant, with the right supports and treatments, most people with a mental health condition can recover and lead fulfilling lives.
There should be emphasis on health ethics and national policy on health 2017 promises for health for all. It envisages for moral and ethical principles in health and the government has efforts in integrating modern medicine with traditional medicines to ensure affordability, quality, reachability and accountability of health system in India.
Spread the Word
